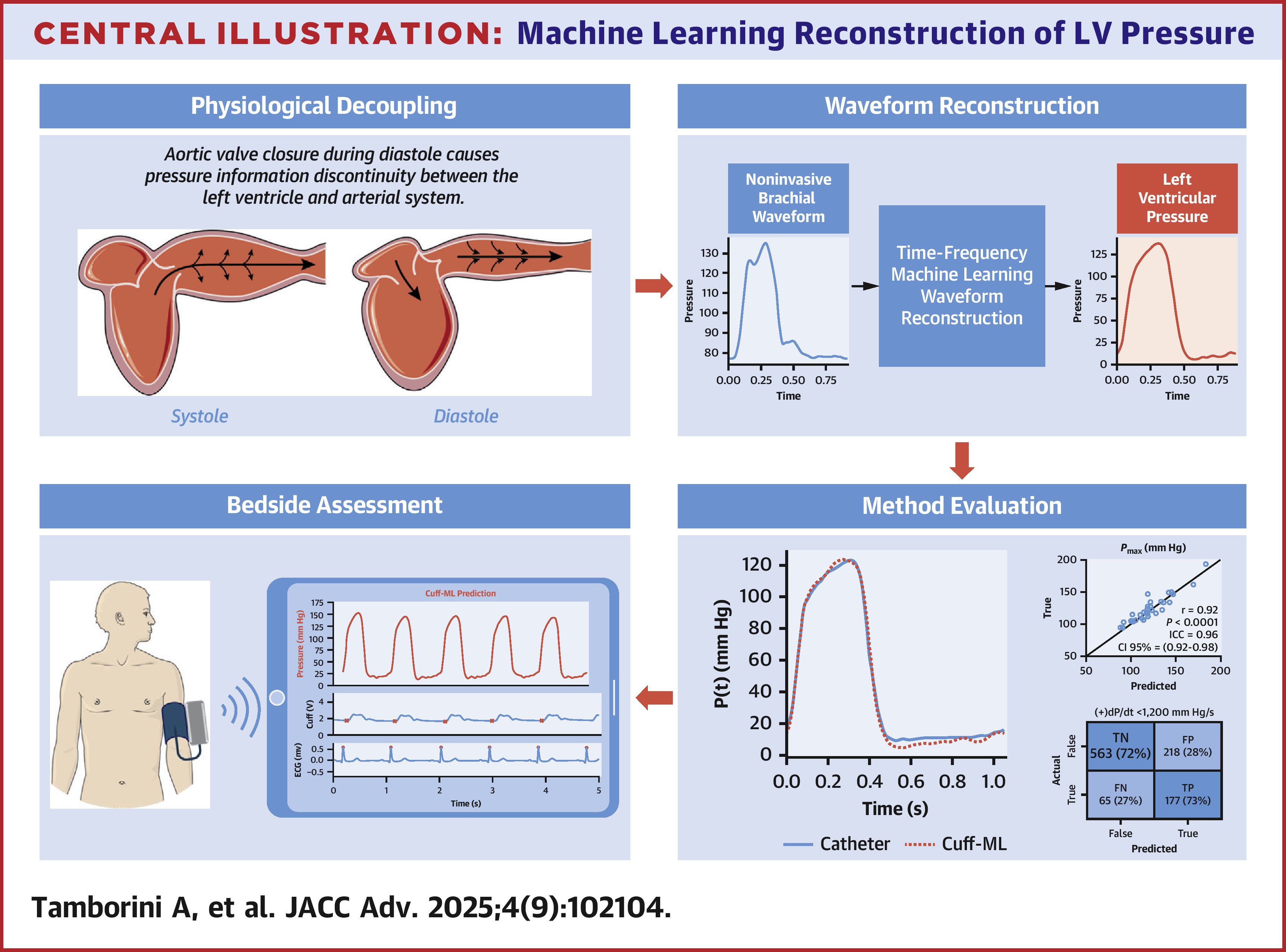
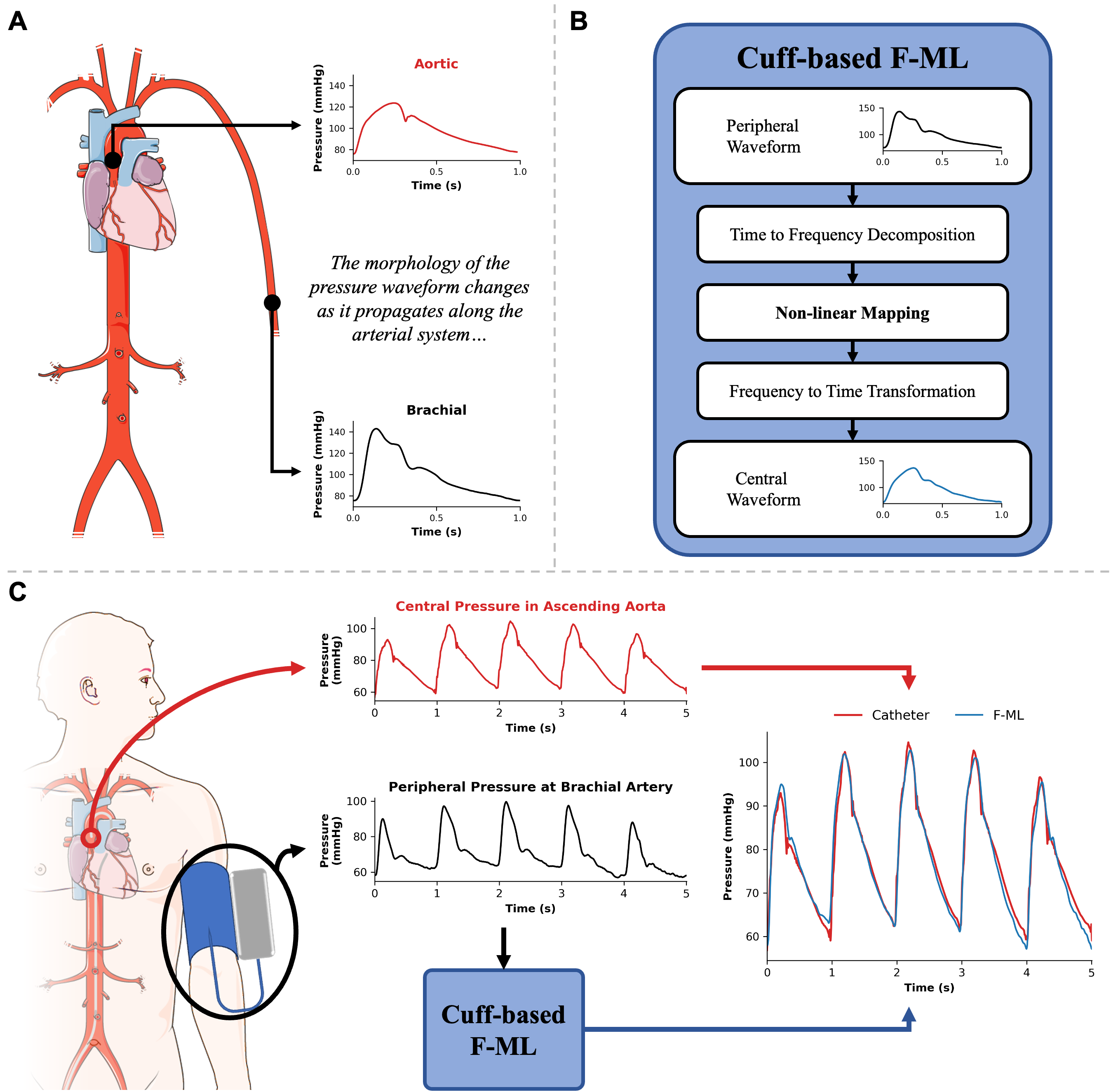
A spectral machine learning approach to derive central aortic pressure waveforms from a brachial cuff
Mapping peripheral to central pressure waveforms offers a promising approach for noninvasive assessment of the aortic pressure waveform. Traditional methods rely on population-based averaging, which fail to account for the complex wave interactions within the arterial system, leading to poor morphological accuracy. This study introduces a wave-based approach that combines brachial cuff measurements with machine learning to nonlinearly map brachial wave components to the aortic site, enabling accurate reconstruction of the central pressure waveform. By accounting for nonlinear wave interactions, this method achieves higher-fidelity waveform reconstruction, improving central pulse wave analysis. Importantly, integration into clinical practice is straightforward, leveraging automated, noninvasive brachial cuff measurements already widely used in healthcare. Analyzing cardiac pulse waveforms offers valuable insights into heart health and cardiovascular disease risk, although obtaining the more informative measurements from the central aorta remains challenging due to their invasive nature and limited noninvasive options. To address this, we employed a laboratory-developed cuff device for high-resolution pulse waveform acquisition and constructed a spectral machine learning model to nonlinearly map the brachial wave components to the aortic site. Simultaneous invasive aortic catheter and brachial cuff waveforms were acquired in 115 subjects to evaluate the clinical performance of the developed wave-based approach. Magnitude, shape, and pulse waveform analysis on the measured and reconstructed aortic waveforms were correlated on a beat-to-beat basis. The proposed cuff-based method reconstructed aortic waveform contours with high fidelity (mean normalized-RMS error = 11.3%). Furthermore, continuous signal reconstruction captured dynamic aortic systolic blood pressure (BP) oscillations (r = 0.76, P < 0.05). Method-derived central pressures showed strong correlation with the independent invasive measurement for systolic BP (R2 = 0.83; B [LOA] = −0.3 [−17.0, 16.4] mmHg) and diastolic BP (R2 = 0.58; B [LOA] = −0.7 [−13.1, 11.6] mmHg). Shape-based features are effectively captured by the spectral machine learning method, showing strong correlations and no systemic bias for systolic pressure–time integral (r = 0.91, P < 0.05), diastolic pressure–time integral (r = 0.95, P < 0.05), and subendocardial viability ratio (r = 0.86, P < 0.05). These results suggest that the nonlinear transformation of wave components from the distal to the central site predicts the morphological waveform changes resulting from complex wave propagation and reflection within the cardiovascular network. The proposed wave-based approach holds promise for future applications of noninvasive devices in clinical cardiology.